Healthcare-Associated Infections - (HAI's)
the culture behind the scenes
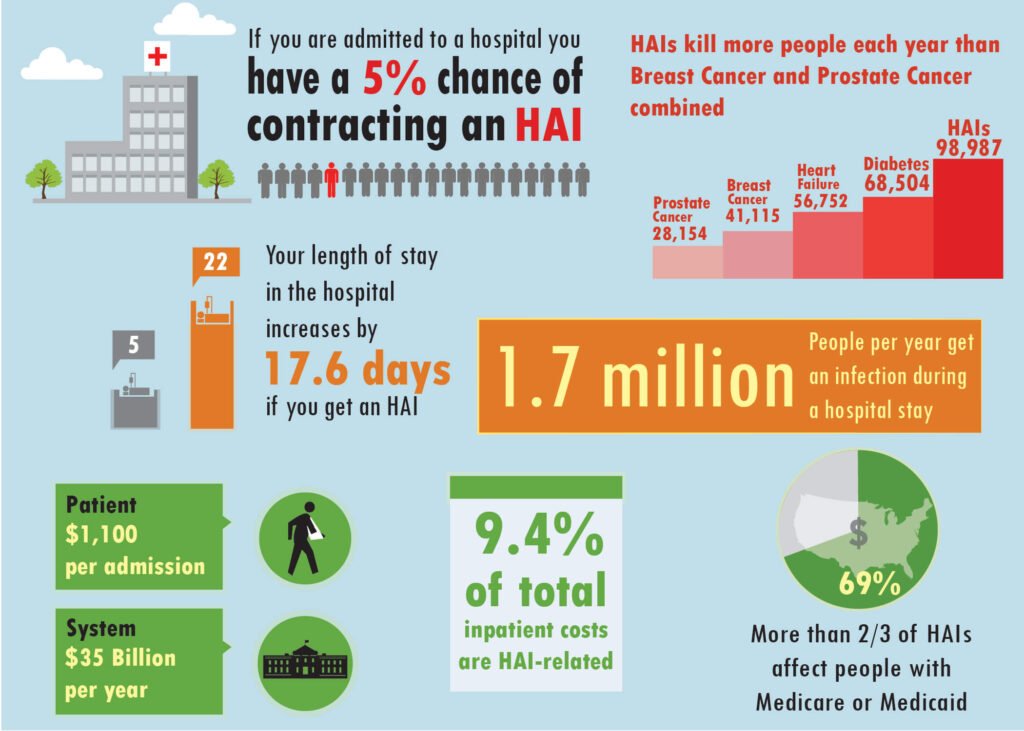
“Healthcare Associated Infections” or “Hospital Acquired Infections” carry the more commonly designated acronym of HAI’s. They all refer to infections which patients contract while under institutional medical care of an unrelated ailment. The contagion can occur while there is treatment being administered for the different illness, or during the time of rest, recovery, and recuperation.
The healthcare facilities in which these infections thrive include emergency rooms, hospitals, nursing homes, long-term care facilities, independent surgical centers, and even local doctors offices’.
Although pneumonia and surgical site infections lead the way within “bloodstream” HAI’s, it is the more avoidable HAI’s which exasperate infectious disease professionals within our healthcare systems. These would relate to the most prevalent “touch transmissible” diseases such as MRSA, Clostridium Difficile (C. Diff), and Vancomycin-resistant Enterococci (VRE).
The most stifling factor about this trio of “touch transmissible” infections is their impregnability,
because of their multi drug-resistant organisms (MDRO) composition.
The second compounding element is that these infections should be more avoidable because they can be better controlled through a properly supervised and regulated hospital personnel “hand cleansing policies” program.
Although a large percentage of healthcare facilities have reluctantly adopted programs to reduce these touch transmissible HAI’s during their personnel’s daily routine practice schedule, very few have netted high success rates.
These infections have long been a major concern to health organizations, including public and private organizations, across the globe. These entities have tried to commit specialized programs to tackle the issues and stigmas, and alter the culture which is tied to noncompliance of hand-hygiene protocols.
While major breakouts seem to garner a lot of focus and media attention for short periods of time, the reality is that these diseases have become endemic within the healthcare systems. Because of this, the impetus should be on raising the success rate against these infections from the 50 to 60% rate where they stand at now, into the 90% tier, not complete elimination.
Unfortunately the lack of compliance, apathetic and complacent work ethic, and the shortage of medical personnel worldwide (healthcare
provider-to-patient ratio) has thwarted these efforts.

MRSA Methicillin-Resistant Staphylococcus Aureus
is a bacterium responsible for difficult-to-treat infections in humans
Methicilin Resistant Staphylococcus Aureus (MRSA), is a type of staph infection that cannot be killed by penicillin or similar antibiotics. Approximately 1 out of every 100 people carries MRSA without making them sick.
MRSA infections occur mostly in hospitals and healthcare facilities; here it can survive anywhere. It can be present and transmissible on numerous surfaces throughout the facilities: patient rooms, access doors, bathrooms, hallways, banisters, and elevators.
“These figures suggest that MRSA infections are responsible for more deaths in the U.S. each year than AIDS.”
A 2007 “Centers for Disease Control and Prevention” (CDC) report, estimated that the number of MRSA infections treated in hospitals had doubled nationwide, from approximately 127,000 in 1999 to 278,000 in 2005, while at the same time deaths increased from 11,000 to more than 17,000.
A 2004 study showed that patients with MRSA infection had, on average, 3X the length of hospital stay (14.3 vs. 4.5 days), incurred 3X the total cost ($48,824 vs $14,141), and experienced 5X the risk of in-hospital death (11.2% vs 2.3%) than those without the infection.
Another study estimated that MRSA would have been responsible for 94,360 serious infections and associated with 18,650 hospital stay-related deaths in the United States in 2005. As is to be expected, these infections are routinely carried outside the healthcare facility walls by unsuspecting visitors, or even hospital personnel.
CA-MRSA
CA-MRSA, Community Acquired MRSA, is the name given to the strand of this disease when it is contracted without any exposure to a recently hospitalized person, usually within the previous 12 months. The symptoms can be manifested as skin infections resembling boils or pimples, and can occur in otherwise healthy people. CDC-investigated clusters have shown that the most common factors linked to the spread of CA-MRSA infections include: cuts or abrasions, skin to skin contact, contaminated items and surfaces, crowded living conditions, and poor hygiene.
“A newer form of staph infection, known as CA-MRSA (Community-Acquired Methicillin Resistant Staphylococcus Aureus), has appeared with increasing frequency, and is now an epidemic within certain community populations.”
The most critical difference between the two types of MRSA is that the community form (CA-MRSA),
possesses a potent toxin called Panton-Valentine Leukocidin, which attacks infection-fighting white blood cells called leukocytes.
The more serious forms of CA-MRSA infection cause necrotizing fasciitis (NF). This can be a severe, rapidly progressing, and life threatening skin infection.
How can a person become infected?
CA-MRSA, MRSA & Staph can be spread when a person: has direct skin-to-skin contact with an infected person, touches surfaces that have staph on them from someone else’s infection (eg: towels, athletic equipment, used bandages). These are not usually passed through the air.
How are Staph and MRSA Infections treated?
Some staph skin infections are treated by draining the sores and may not require antibiotics. Draining these sores should be done by a doctor. If the doctor gives you antibiotics, make sure you take all of the medicine, even if the infection is getting better. Do not share your medicine with anyone else or save it to use at another time. Call your doctor back if the infection does not get better after a few days. If other people you know or live with get the same infection tell them to go to their doctor.
What do Staph and MRSA Infections look like?
Common skin conditions caused by Staph and MRSA may look like any of the following:
- Sores that look and feel like spider bites. (but are not spider bites) Red painful bumps under the skin called boils or abscesses.
- A cut that is swollen, hot, and filled with pus.
- Blisters filled with fluid or red skin with a honey-colored crust (usually on the face).
- Red, warm, firm skin area that is painful and getting larger (usually on the legs).



Signs and Symptoms
- Cellulitis – an infection of the skin or the fat and tissue directly beneath the skin. Usually starts as small rednbumps.
- Boils – a pus-filled infection in the hair follicles of the skin.
- Abscesses – collections (one or more) of pus under the skin.
- Carbuncles – infections larger than an abscess, usually with several openings to the skin.
- Impetigo – a skin infection with pus-filled blisters.
Preventing MRSA and Staph Infections:
Hand-hygiene, including handwashing and the supplemental use of alcohol-based hand cleansers, is the easiest way to
prevent MRSA and Staph Infections.
When practicing hand-hygiene?
- Whenever the skin comes into contact with other people or with shared surfaces or equipment
- Before and after athletic practice, games, or working out
- After sneezing, coughing, blowing or touching the nose
- Before and after touching the eyes, nose, or mouth, or skin that has open sores, boils, and skin rashes
- After using the toilet or urinal
- After touching any item soiled with wound fluids, such as bandages, dressings, or bedding
- After cleaning the bathroom, changing your bedding, doing laundry; and before preparing food, eating, or drinking
- If soap and running water is not available and hands do not have visible dirt on them, staph germs can be killed by using alcohol-based hand cleansers
For more information: http://www.cdc.gov